How do CMS Quality Scores Affect Your Plan?
CMS recently published the 2023 Medicare Advantage and Part D Star ratings, which showed
an overall decrease in average Star ratings across the board, especially compared to the record high ratings seen in 2022 – thanks to the relaxed standards and methodology changes implemented during the pandemic. Now that these guardrails or disaster provisions have been removed and more stable cut points have been put in place, the backdrop is more challenging for health plans as the percentage of members in 4+ Star plans in 2024 will likely be the lowest it’s been in several years. This prompts a call to action for health plans looking to succeed in delivering high-quality, affordable, and coordinated care to their members in this evolving landscape and to improve and sustain Star ratings on a go forward basis.
Why it Matters
In 2022, there are more than 28 million people enrolled in a Medicare Advantage plan, a number that is expected to grow significantly as the number of 65+ individuals continues to grow and as a greater percentage of these eligible Medicare beneficiaries choose to enroll in Medicare Advantage plans. To capture this demand, it has become increasingly important to for health plans to focus on improving and sustaining their Star ratings year over year, especially given the financial and marketing benefits that come with obtaining a 4+ Star plan as well as the ability to attract membership growth.
Stellar Solution
Stellar Health improves Star ratings by engaging primary care physicians (PCPs) to act on quality metrics at the point of care when the patient is in the office and to proactively engage patients for annual visits. Stellar offers real-time recognition and monthly payment to PCPs as gaps are closed. Specifically, our solution supports numerous quality measures, including but not limited to Part C & Part D measures related to medication adherence, preventative screenings, and diabetes care.
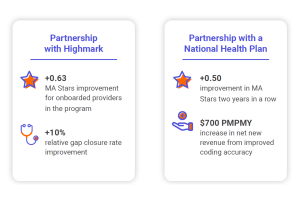
Demonstrating Success
How can we help you?
- View a product demo
- Schedule a meeting
- Partner with us

